Sickle cell disease (SCD) is an inherited red blood disorder that leads to acute episodes of worsening hemolysis and vaso-occlusion. The clinical course of these exacerbations can be unpredictable and some patients have rapid clinical deterioration requiring care in the intensive care unit (ICU). The utility of the Acute Physiology and Chronic Health Evaluation (APACHE II) score to predict ICU outcomes is unclear.
We investigated the etiologies and outcomes in SCD patients requiring admission to the ICU at our institution, and the ability of the APACHE II score to predict length of stay (LOS) and mortality. Subjects were identified from a prospective registry of 439 SCD patients and baseline clinical data was obtained at the time of enrolment into the registry. The APACHE II score was calculated using the worst physiologic values measured within 24 hours of admission to the ICU. Linear and categorical variables were compared by the Kruskall-Wallis and chi-square test, respectively, and median (interquartile [IQR]) values are provided.
Between 1/2008 and 2/2020, 134 (31%) SCD patients required 338 ICU admissions over a median follow up time of 8.8 years after enrollment into the registry (IQR, 6.5 - 9.4 years). SCD patients that required an ICU admission had higher median systolic blood pressure (122 vs. 117 mmHg, P=0.004) and white blood cell count (10.3 vs. 9.5 x 103/uL, P=0.09) and lower median estimated glomerular filtration rate (123 vs. 134 mL/min/1.73m2, P=0.02) at entry into the registry compared to those that did not require admission to the ICU during the follow-up period. After adjusting for age, sex, hydroxyurea use and SCD genotype, a higher baseline systolic blood pressure was independently associated with risk of ICU admission by logistic regression analysis (OR 9.3 for each natural log increase in blood pressure, 95%CI 1.3-67.5; P=0.03).
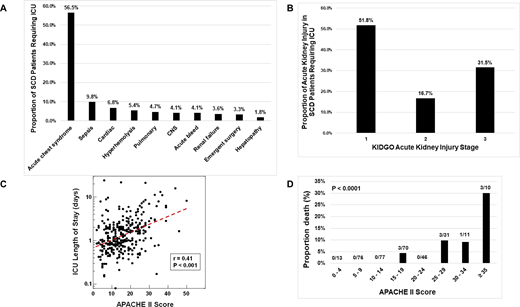
The median age at the time of ICU admission was 40 years (IQR, 27 - 50 years); 53% of the patients were female, 78% had Hb SS/Sβ0-thalassemia genotype, and 48% were on hydroxyurea therapy. Acute chest syndrome was the most common cause of admission to the ICU, representing 57% of the cases (Figure 1A). While in the ICU, 19.2% required ventilation support (8% mechanical ventilation, 11.2% bilevel positive airway pressure) and 6.2% required vasopressor support. Acute kidney injury, as defined by the KDIGO guidelines, was observed in 33.7% of ICU admissions (Figure 1B) and 4.1% required acute initiation of renal replacement therapy. Acute thrombosis occurred in 5.1% of ICU SCD patients (1.5% deep vein thrombosis, 3.6% pulmonary emboli).
While in the ICU, the median LOS was 1.1 days (IQR, 0.7 - 2.0 days) and 10 deaths occurred (3% of ICU admissions). The median APACHE II score was 15 (IQR, 9-21) and the score was directly associated with ICU LOS (r=0.41, P<0.0001) (Figure 1C) and a higher risk for death (OR 2.2 for each age-adjusted 5-point increment, 95%CI: 1.5-3.4; P=0.0002) (Figure 1D). An exchange transfusion was performed in 126 (37.3%) of the ICU admissions. Mortality was 0.8% in patients not receiving an exchange transfusion versus 4.3% in those not receiving exchange (P=0.07). After adjusting for age and APACHE II score, the odds ratio of death in patients receiving an exchange transfusion was 0.12 (95%CI 0.01 - 1.26; P=0.08).
In conclusion, we demonstrate that approximately one-third of SCD patients require ICU care and that acute chest syndrome is the most common reason. Despite frequent requirement for vasopressor, ventilation or renal support, the mortality rate was low at 3%. This rate is substantially lower than the 8 - 19% mortality rate observed in general ICU admissions. The APACHE II score, a tool that predicts ICU outcomes, was predictive of LOS and risk of death in our SCD cohort. Furthermore, exchange transfusion was associated with a trend of lower mortality. Future studies on clinical predictors of ICU admissions and outcomes could help clinicians anticipate sickle cell complications and mortality and encourage early intervention such as the use of exchange transfusion.
Gordeuk:Ironwood: Research Funding; Imara: Research Funding; CSL Behring: Consultancy, Research Funding; Global Blood Therapeutics: Consultancy, Research Funding; Novartis: Consultancy. Saraf:Global Blood Therapeutics: Membership on an entity's Board of Directors or advisory committees, Other: Advisory Boards, Speakers Bureau; Pfizer, Global Blood Therapeutics, Novartis: Research Funding; Novartis, Global Blood Therapeutics: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal